A CDC food safety alert regarding a multistate outbreak of Salmonella Typhimurium infections has been posted: https://www.cdc.gov/salmonella/typhimurium-07-21/index.html
Eight people infected with the outbreak strain of Salmonella Typhimurium have been reported from two states (Wisconsin and Illinois). No hospitalizations or deaths have been reported.
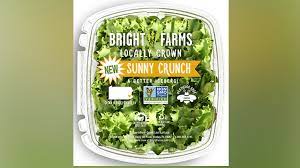
Interviews with ill people and traceback information show that BrightFarms brand Sunny Crunch salad may be contaminated with Salmonella and making people sick. At least five people ate or bought this product before getting sick.
The true number of sick people in an outbreak is likely higher than the number reported, and the outbreak may not be limited to the states with known illnesses. This is because some people recover without medical care and are not tested for Salmonella.
Investigators are working to identify if additional products are contaminated.
CDC is advising people not to eat, sell, or serve BrightFarms brand Sunny Crunch salad. See the Food Safety Alert for product details and description.
What You Should Do:
Do not eat, sell, or serve BrightFarms brand Sunny Crunch salad produced in Rochelle, IL. Throw it away or return it to where you bought it. Even if some of the salad was eaten and no one got sick, throw the rest away or return it.
Wash items and surfaces that may have touched the salad using hot soapy water or a dishwasher.
Contact a healthcare provider if you think you got sick from eating the salad.
About Salmonella:
Most people infected with Salmonella develop diarrhea, fever, and stomach cramps 6 hours to 6 days after being exposed to the bacteria.
The illness usually lasts 4 to 7 days, and most people recover without treatment.
In some people, the illness may be so severe that the patient is hospitalized. Salmonella infection may spread from the intestines to the bloodstream and then to other parts of the body.
Children younger than 5, adults 65 and older, and people with weakened immune systems are more likely to have severe illness.
If you have questions about cases in a particular state, please call that state’s health department.