Joshua Mansour, M.D., a board-certified hematologist and oncologist in Stanford, California doing work in the field of hematopoietic stem cell transplantation and cellular immunotherapy (left, exactly as shown), writes in this contributed piece, from the beginning of medical school, one of the first things instructional videos that we had to watch during orientation was about social media and what not to do. There began this stigma and it was frowned upon to use social media if you were a healthcare provider.
 There are the obvious things that physicians should not do, such as post private information about patients, show a patient’s face without their permission, or exploit medically sensitive information. But no one tells you what you can do and possibly what you actually should do.
There are the obvious things that physicians should not do, such as post private information about patients, show a patient’s face without their permission, or exploit medically sensitive information. But no one tells you what you can do and possibly what you actually should do.
There is a new wave that has now taken over that we as a healthcare community and a community as a whole should support, especially if it is meant to help others. Most recently I have approached social media in a different way and gone out to explore what is available as a tool to help others. What I’m finding has been mind-blowing and I am very excited to see where it continues to progress in the future.
People are sharing their journeys, inspiring others, raising awareness. There is a whole community of individuals working as a team to help others. It is incredibly inspiring.
Before recently I had thought of social media as being full of people only posting pictures of fun trips or nights out, throwing out their opinions out into the open for people to see. We now have social impact movements, live videos with question and answers for students, people showing their tough times and how they are overcoming them. People are reaching out to others for encouragement, collaborations, and progress. Using it to spread the message. With the busy days of many healthcare professionals, it is difficult for them to find the time to engage with social media and with others. There are many healthcare providers that are making an impact and finding the time to do it.
What we need to start teaching in medical school and in other schools in not only what not to do on social media, but how to use social media in a positive light. This is something that is happening and only continuing to grow. It is time to get on board but shine the light in a positive manner. Teach students from early what to do instead of only what not to do. You never know they may be able to influence people in a way like never before.
Recently I have recently been able to connect with others across the world and learn new things about medicine and how it is practiced in those locations. This will help me evolve as a physician as well and has helped my patients.


 foodservice professional and having to wear medical identification jewelry myself, it’s sad that the only piece of jewelry approved to be worn by foodservice professionals working in kitchens is a plain band ring.
foodservice professional and having to wear medical identification jewelry myself, it’s sad that the only piece of jewelry approved to be worn by foodservice professionals working in kitchens is a plain band ring.  to them any vital information when time is crucial. It is important that hiring/HR managers as well as employees are aware of these alternatives because they can be the difference between life and death. EMTs serve as a means for people to get access to medical care in times when they are in most desperate need for it—help them save a life by informing managers and employees on the alternatives.
to them any vital information when time is crucial. It is important that hiring/HR managers as well as employees are aware of these alternatives because they can be the difference between life and death. EMTs serve as a means for people to get access to medical care in times when they are in most desperate need for it—help them save a life by informing managers and employees on the alternatives..jpg) Olympics? – and OK when the Canadian men won gold, but I still say Vancouver is a dump of a town. Always has been.
Olympics? – and OK when the Canadian men won gold, but I still say Vancouver is a dump of a town. Always has been.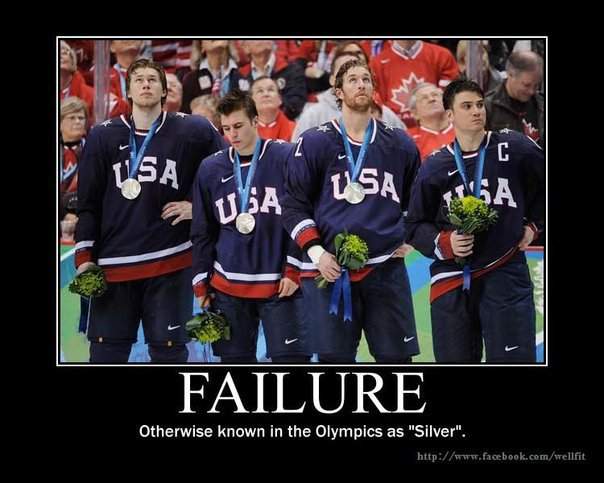
 cuisine comes from the operating room: medical tweezers. In some of the country’s most ambitious restaurants, a pair of them allows a chef to put the final, seemingly impossible touches on a dish.
cuisine comes from the operating room: medical tweezers. In some of the country’s most ambitious restaurants, a pair of them allows a chef to put the final, seemingly impossible touches on a dish. Technically, the Ganja Gourmet is a medical marijuana dispensary, one of many that have sprung up this year throughout Colorado.
Technically, the Ganja Gourmet is a medical marijuana dispensary, one of many that have sprung up this year throughout Colorado.