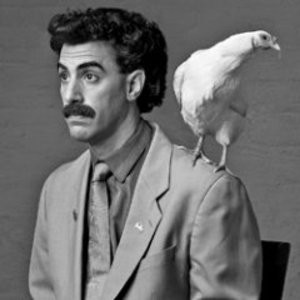
I’ve said it many times before, and will say it again: Stop cuddling your chicks.
The backyard chicken kind.
The U.S. Centers for Disease Control (CDC) and multiple states are investigating several multistate outbreaks of Salmonella infections linked to contact with live poultry in backyard flocks.
Several different types of Salmonella bacteria have made people sick: Salmonella Seftenberg, Salmonella Montevideo, Salmonella Infantis, Salmonella Enteritidis, Salmonella Indiana, and Salmonella Litchfield.
As of June 1, 2018, 124 people infected with the outbreak strains of Salmonella have been reported from 36 states.
Illnesses started on dates ranging from February 2, 2018 to May 14, 2018.
21 ill people have been hospitalized, and no deaths have been reported.
31% of ill people are children younger than 5 years.
Epidemiologic, traceback, and laboratory findings link these outbreaks to contact with live poultry, such as chicks and ducklings, which come from multiple hatcheries.
In interviews, 55 (74%) of 74 ill people with information available reported contact with chicks or ducklings in the week before their illness started.
People reported obtaining chicks and ducklings from several sources, including feed supply stores, websites, hatcheries, and from relatives.
Seventy outbreaks of Salmonella infections have been linked to contact with backyard flocks since 2000[PDF – 887KB]. In 2017, CDC reported the largest number of illnesses ever recorded linked to backyard flocks.
People can get sick with Salmonella infections from touching live poultry or their environment. These birds can be carrying Salmonella bacteria but appear healthy and clean and show no signs of illness.
Follow these tips to stay healthy with your backyard flock:
Always wash hands thoroughly with soap and water right after touching live poultry or anything in their environment.
Don’t let children younger than 5 years handle or touch live poultry without adult supervision.
Set aside a pair of shoes to wear while taking care of your birds and keep those outside of your home.
Do not let live poultry inside the house, in bathrooms, or especially in areas where food or drink is prepared, served, or stored, such as kitchens or outdoor patios.
For a complete list of recommendations, visit the Healthy Pets, Healthy People website section on backyard poultry
And don’t sleep with your chicks.