Trafficking in fake and substandard food is big business, and efforts to stop this global phenomenon are ongoing
 Rotten meat, chemically coloured tuna and fake baby milk powder – these are just a small sampling of the products seized as part of the latest OPSON investigation into the presence of counterfeit and substandard food and beverage products on the market in Europe and beyond.
Rotten meat, chemically coloured tuna and fake baby milk powder – these are just a small sampling of the products seized as part of the latest OPSON investigation into the presence of counterfeit and substandard food and beverage products on the market in Europe and beyond.
Run over the course of 4 months (December 2017 – March 2018) across 67 countries*, OPSON VII resulted in the total seizure of more than 3 620 tonnes and 9.7 million litres of either counterfeit or substandard food and beverages as a results of more than 41 000 checks carried out at shops, markets, airports, seaports and industrial estates. In total some 749 people were arrested or detained with investigations continuing in many countries.
“The results of OPSON demonstrate what can be achieved to protect consumers worldwide when law enforcement agencies join their efforts and perform coordinated actions”, said Jari Liukku, Head of Europol’s European Serious and Organised Crime Centre, “It is a threat which requires such cooperation across borders, taking into account the increased integration and globalisation of supply chains. All countries face this threat and it is the duty of law enforcement agencies to make sure what consumers get in their plate is genuine and safe”.
“The dismantling of nearly 50 criminal networks involved in the production of fake food and drink is an important result in stemming the flow of potentially lethal products into the marketplace,” said Daoming Zhang, Head of INTERPOL’s Illicit Markets unit. “The volume of counterfeit and substandard products seized is a reminder to the public that they need to remain careful about what they buy and from where.”
The annual operation coordinated by Europol and INTERPOL is supported by customs, police and national food regulatory bodies in addition to partners from the private sector. Since its first edition in 2011, the number of countries taking part in OPSON has grown every year, reflecting the growing commitment to tackle this issue.
In Europe the close cooperation established between Europol and the EU Commission coordinating the EU Food Fraud Network led to the implementation of a specific project targeting the fraudulent trade of tuna. A comprehensive approach involving all stakeholders allowed the phenomenon to be tackled in an innovative and more effective manner via the simultaneous use of administrative and criminal enforcement tools. Europol will continue to support this multiagency approach in the upcoming editions of OPSON.
Belgium – sale of rotten meat unfit for consumption
Belgium closed a major meat processing plant in the country, and supermarkets have taken meat products off their shelves in a scandal over rotten meat. The incriminated company saw its licence revoked by the federal government, after spot checks revealed a potential health risk in two products: minced beef and oxtail. Officials found traces of so-called meat waste, pieces of the carcass, intended for animal feed which are prohibited for human consumption.
Spain – fake baby milk powder
Four people have been arrested and a factory that packaged counterfeit baby milk mostly destined for China dismantled in Spain. Eight tonnes of the forged product were seized. The powder bought in bulk in Poland for one euro per kilo and delivered to Barcelona was not harmful but it lacked the nutrients needed by infants. It was also made in an environment that did not comply with food health and safety standards.
European wide-action – fraudulent practices in the tuna fish industry
During OPSON VII, an EU coordinated action was run with the support of the EU Food Fraud Network across 11 European countries** in order to detected fraudulent practices pertaining to tuna fish. This was the first time that such an action was carried out on a specific product. The illicit practises included species substitution and fraudulently selling tuna intended for canning as fresh. In this case, the tuna intended for canning was illegally treated with chemical substances that altered its colour to give the misleading impression of its freshness. In total, more than 51 tonnes of tuna were seized and more than 380 samples were taken.
France- smuggling of perishable goods
In a joint operation, The French Gendarmerie, Customs, Police and Ministry of Agriculture seized in its overseas territories over 9.5 tonnes of smuggled perishable goods and 60 litres of fuel and raw material intended for illegal gold mining.
Training in the detection of food fraud
Throughout the year, representatives from a variety of agencies and sectors – police and customs officers, prosecutors, investigative experts – attend training courses and workshops in advance of the operational activity. These hands-on workshops equip participants with the knowledge they need for the raids and follow-up investigations, in particular, enabling them to better distinguish fake products from genuine ones. In Hungary, the National Tax and Customs Administration in cooperation with the National Food Chain Safety Office and the National Board Against Counterfeiting produced a short video to explain the operation to law enforcement officers and a general audience.
A final and detailed report on the results of the operation OPSON VII will be published in the upcoming months.
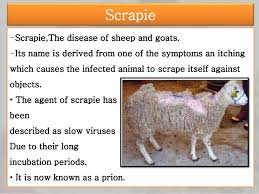 This report presents the results of surveillance on transmissible spongiform encephalopathies (TSE) in cattle, sheep, goats, cervids and other species, and genotyping in sheep, carried out in 2019 by 28 Member States (MS), and by Iceland, Montenegro, North Macedonia, Norway, Serbia and Switzerland (non‐MS).
This report presents the results of surveillance on transmissible spongiform encephalopathies (TSE) in cattle, sheep, goats, cervids and other species, and genotyping in sheep, carried out in 2019 by 28 Member States (MS), and by Iceland, Montenegro, North Macedonia, Norway, Serbia and Switzerland (non‐MS).