The Public Health Agency of Canada (PHAC) really sucks at this communication thing. They sucked during the 2008 Listeria outbreak linked to Maple Leaf cold cuts that killed 24 and sickened a further 33, they have always sucked when discussing numerous outbreaks of Cyclospra, and I guess they realized they suck so bad they didn’t even try during an outbreak spanning 2015-2016 linked to Listeria in milk.
 Now, over three years since residents of Ontario (that’s in Canada) began reporting illnesses from Listeria in pasteurized chocolate milk produced at a dairy in Georgetown, Ontario, investigators have gotten around to saying just how many people got sick.
Now, over three years since residents of Ontario (that’s in Canada) began reporting illnesses from Listeria in pasteurized chocolate milk produced at a dairy in Georgetown, Ontario, investigators have gotten around to saying just how many people got sick.
According to health-types writing in Emerging Infectious Disease, 11 case-patients had an onset date during November 14, 2015–February 14, 2016. Onset dates ranged from April 11 to June 20, 2016, for 21 case-patients in the second wave; the remaining 2 case-patients were outliers. Median age was 73 years (range <1 years–90 years). More than half of the case-patients were female (20/34, 59%). Hospitalizations occurred for 32 (94%) case-patients, and 4 deaths (12%) were reported.
In Ontario, local public health professionals complete the national invasive listeriosis questionnaire and collect food samples. We conducted a case–case analysis by using Ontario case-patients listed in the national listeriosis database as controls. We used a variety of methods to support hypothesis generation, including supplemental questionnaires, centralized interviewing, and reviewing purchase records collected through shoppers’ loyalty card programs. A meeting was also held with representatives from a grocery chain that was common for case-patients (retail chain A) for insights into possible sources.
PFGE and whole-genome sequencing were performed at the Public Health Ontario Laboratory, in accordance with PulseNet Canada protocols (Table). Food safety investigations, including targeted retail sampling, were conducted by the Canadian Food Inspection Agency and Ontario Ministry of Agriculture and Food and Rural Affairs. Laboratory analyses of food samples were conducted by the Canadian Food Inspection Agency and the Public Health Ontario Laboratory.
Several hypotheses were generated during the course of this outbreak. In the first wave, a concurrent listeriosis outbreak associated with leafy greens was ongoing in the United States and Canada. However, product testing did not establish a relationship between the 2 outbreaks. Cheddar cheese was also suspected, but a food safety investigation, including sampling at the manufacturer, did not support a link to this outbreak (6,7). Although leafy greens and cheddar cheese were ruled out, 1 commonality remained; shopping at retail chain A was reported frequently by case-patients.
A second wave began in April 2016 in which 10 of 17 case-patients reported consuming coleslaw. Six case-patients ate coleslaw from the same manufacturer, which supplied retail chain A and a fast food restaurant chain. However, the food safety investigation, including sampling at the manufacturer and supplier, did not support this hypothesis.
On May 24, 2016, L. monocytogenes isolated from expired bagged chocolate milk collected from the home of 1 case-patient was confirmed to have the outbreak strain PFGE pattern. Fluid milk in Canada is often sold in plastic bags. In this instance, the outer packaging, which is the only area that contains the brand name, was discarded. Thus, the brand name was uncertain, and efforts were undertaken to confirm the source of the chocolate milk. Because the proxy of the case-patient reported purchasing brand B milk, samples of brand B chocolate and white milk were collected from retail for testing. Brand B was the main brand of chocolate milk sold by retail chain A, and it is distributed only in Ontario.
Although the hypothesis-generating questionnaire used stipulated milk, with flavored milk as a prompt, chocolate milk was not specified, and as a result this type of milk might have been underreported. Exposure to pasteurized milk was reported by 60% of case-patients in the first wave compared with 76% of controls. Thus, milk was not originally pursued as a source. However, this new positive isolate led to re-interviewing of case-patients from the second wave and resulted in 9 (75%) of 12 case-patients reporting consuming brand B when asked specifically about chocolate milk.
On June 3, a retail sample of brand B chocolate milk was confirmed positive for L. monocytogenes. This finding led to a class I recall of 1 lot of brand B chocolate milk. On June 5, the recall was expanded to all lots of brand B chocolate milk processed at that facility because of the result of extensive retail sampling. Isolates from the original sample and 3 subsequent positive samples of chocolate milk matched the outbreak strain by PFGE and whole-genome sequencing. No white milk samples were positive for L. monocytogenes.
Environmental sampling at the manufacturer confirmed the presence of the outbreak strain within a post-pasteurization pump dedicated to chocolate milk and on nonfood contact surfaces. This post-process contamination of the chocolate milk line was believed to be the root cause of the outbreak. A harborage site might have been introduced by a specific maintenance event or poor equipment design. The equipment was subsequently replaced, and corrective measures were implemented to prevent reoccurrence. Chocolate milk production was resumed after vigorous testing for L. monocytogenes under regulatory oversight.
Conclusions
This outbreak lasted 7 months and resulted in 34 confirmed listeriosis case-patients. Discovering the cause of this listeriosis outbreak was challenging because pasteurized chocolate milk is a commonly consumed product. Although there have been previous outbreaks outside Canada caused by chocolate milk, pasteurized milk products are generally not expected to be the source. This outbreak highlights that even pasteurized products can be contaminated by and support the proliferation of L. monocytogenes when contamination is introduced post-pasteurization. The possibility of post-processing contamination indicates an ongoing need for regulatory oversight and robust quality assurance processes, which include routine sampling of the environment and finished products.
Brand B chocolate milk is a widely distributed product in Ontario, and contamination of this product could have resulted in >34 case-patients. It is possible that a lower number of case-patients were reported because chocolate milk may primarily be consumed by younger, healthier persons, in whom invasive listeriosis is less likely to develop. Another possible explanation is that the contamination in the milk appeared to be intermittent, with some samples testing positive while others tested negative. As such, careful attention should be given to equipment design and maintenance programs, as harborage sites could result in recurring contamination that goes undetected by routine monitoring. Targeted retail and environmental sampling was instrumental in identifiying the root cause in the facility and the breadth of potentially implicated products in the marketplace. Thus, this type of sampling should be considered during outbreak investigations.
 Ultimately, the implicated product was determined on the basis of testing of food items obtained from the home of 1 case-patient. This finding highlights the necessity of obtaining a thorough food history and collecting and testing available samples of food that case-patients consumed during the incubation period. In Canada, where bagged milk is common, labeling of the inner and outer bags with the brand name would facilitate product identification by consumers. This recommendation could extend to other food products in North America (e.g., frozen hamburger patties) that have multiple layers of packaging.
Ultimately, the implicated product was determined on the basis of testing of food items obtained from the home of 1 case-patient. This finding highlights the necessity of obtaining a thorough food history and collecting and testing available samples of food that case-patients consumed during the incubation period. In Canada, where bagged milk is common, labeling of the inner and outer bags with the brand name would facilitate product identification by consumers. This recommendation could extend to other food products in North America (e.g., frozen hamburger patties) that have multiple layers of packaging.
That is a lucid, thought provoking summary of a complex foodborne outbreak, fraught with uncertainties.
When the Canadian Food Inspection Agency announced the recall on June 4, 2016, Chapman wrote it up for the blog, reminiscing about his childhood innocence in southern Ontario, and noted, as has become the pattern, that CFIA reports recalls, but it’s up to PHAC or provincial health ministries to identify the number of sick people. As far as I can tell, no public statement about illnesses was ever made, until now.
What the fuck do these people do, especially the communication hacks? Do they have a responsibility to the public? Why didn’t epidemiology count and a public warning issued rather than waiting for a positive sample in an unopened package, which has apparently become the Canadian standard for going public?
If that’s the standard, that sucks.
Listeria monocytogenes associated with pasteurized chocolate milk, Ontario, Canada
March 2019
Emerging Infectious Diseases vol. 25 no. 3
Heather Hanson , Yvonne Whitfield, Christina Lee, Tina Badiani, Carolyn Minielly, Jillian Fenik, Tony Makrostergios, Christine Kopko, Anna Majury, Elizabeth Hillyer, Lisa Fortuna, Anne Maki, Allana Murphy, Marina Lombos, Sandra Zittermann, Yang Yu, Kristin Hill, Adrienne Kong, Davendra Sharma, and Bryna Warshawsky
https://wwwnc.cdc.gov/eid/article/25/3/18-0742_article
In an investigation of a listeriosis outbreak in Ontario, Canada, during November 2015–June 2016, Public Health Ontario identified pasteurized chocolate milk as the source. Because listeriosis outbreaks associated with pasteurized milk are rare in North America, these findings highlight that dairy products can be contaminated after pasteurization.

(2)(1).jpg) “Several of the students who had just eaten a meal at the dining hall became ill,” she said. “We’ve told the university we can’t rule out the possibility that food was related to the outbreak, in addition to person-to-person transmission.”
“Several of the students who had just eaten a meal at the dining hall became ill,” she said. “We’ve told the university we can’t rule out the possibility that food was related to the outbreak, in addition to person-to-person transmission.”(2).jpg) University spokesperson Julie Bataille said,
University spokesperson Julie Bataille said, That’s the same Stephanie Sampiere who was quick off the mark when I published an entry about a
That’s the same Stephanie Sampiere who was quick off the mark when I published an entry about a .jpg) Georgetown officials were also cited as saying today that:
Georgetown officials were also cited as saying today that:
.jpg) After striking
After striking 
 My hockey bag is still filled with those little soaps and shampoos from hotel rooms around the globe.
My hockey bag is still filled with those little soaps and shampoos from hotel rooms around the globe.
 However, the reporters at the
However, the reporters at the .jpg) UPDATES: Todd Olson says the new number is 175 students. Only 3 in emergency room, 2 in student health center.
UPDATES: Todd Olson says the new number is 175 students. Only 3 in emergency room, 2 in student health center.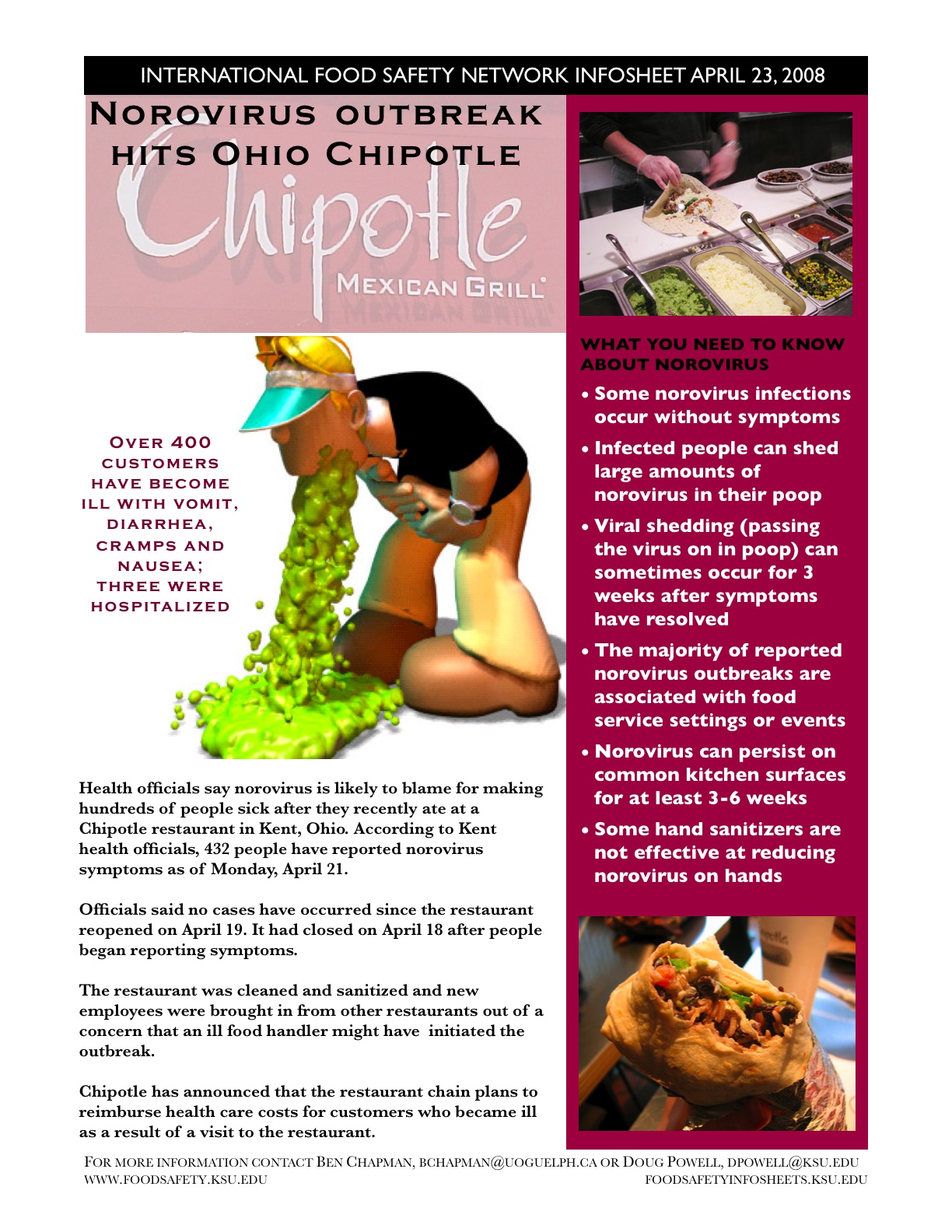
 At least 96 students were treated by the Georgetown University Hospital or the Student Health Center for gastroenteritis from Tuesday night and Wednesday. …
At least 96 students were treated by the Georgetown University Hospital or the Student Health Center for gastroenteritis from Tuesday night and Wednesday. …-1.jpg) The actual number of students who have fallen ill may be far higher than reported. Interviews have revealed that many students who fell ill did not get medical help, like Katie O’Niell (COL `11), who began to vomit about three hours after eating a burrito at Leo’s.
The actual number of students who have fallen ill may be far higher than reported. Interviews have revealed that many students who fell ill did not get medical help, like Katie O’Niell (COL `11), who began to vomit about three hours after eating a burrito at Leo’s. Any food service operation is vulnerable to foodborne illness, but the university ones have been popping up regularly of late –
Any food service operation is vulnerable to foodborne illness, but the university ones have been popping up regularly of late –