Another nugget from the European Commission’s Rapid Alert System for Food and Feed.
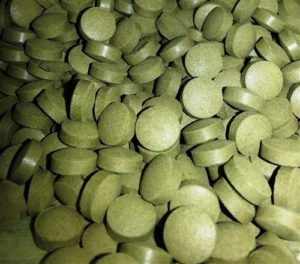 Shiga toxin-producing Escherichia coli (stx1+; O145 /25g) in organic wheatgrass tabletts from Germany
Shiga toxin-producing Escherichia coli (stx1+; O145 /25g) in organic wheatgrass tabletts from Germany
Seriously, organic wheat grass tablets?

Another nugget from the European Commission’s Rapid Alert System for Food and Feed.
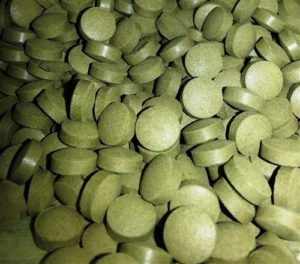 Shiga toxin-producing Escherichia coli (stx1+; O145 /25g) in organic wheatgrass tabletts from Germany
Shiga toxin-producing Escherichia coli (stx1+; O145 /25g) in organic wheatgrass tabletts from Germany
Seriously, organic wheat grass tablets?
A Minnesota high school science project that involved hunting and butchering deer — including one road-kill capture — and turning the meat into venison kabobs backfired when 29 students were sickened with a rare kind of E. coli food poisoning, investigators say.
Linda Carroll of msnbc reports the 2010 incident, just now reported in the journal Emerging Infectious Diseases (abstract below) highlights the risks of E. coli contamination, not just from factory-produced meat, but also from small, local providers.
Doctors first knew they had a problem in December 2010 when two kids from the same high school turned up at a Minnesota hospital with abdominal pain and bloody diarrhea. Fearing they  had a food poisoning outbreak on their hands, they quickly called in the state’s top-notch public health officials.
had a food poisoning outbreak on their hands, they quickly called in the state’s top-notch public health officials.
Both teens had taken part in a school environmental science and outdoor recreation class that involving hunting, shooting and butchering six white-tailed deer, explained Joshua Rounds, the study’s lead author and an epidemiologist with the Minnesota Department of Public Health. A seventh deer was harvested after being hit by a car, the report says.
The deer were processed on school grounds and then grilled and eaten in class a few weeks before the students got sick.
Epidemiologists interviewed 117 kids in five class periods and found that 29 definitely had become ill, but not with E. coli O157:H7, the strain commonly associated with food poisoning from ground beef.
Rounds suspected the deer might have carried another E. coli strain that also produces poisons known as Shiga toxins. He was right. Samples from the students and the deer meet turned up E. coli O103:H2, which is part of a larger category of non-O157 Shiga toxin-producing E. coli bugs, known as STECs.
Scientists also turned up another E. coli strain, E. coli O145:NM that didn’t produce Shiga toxins.
People don’t usually get sick from eating hunks or steaks of muscle meat, Rounds said. In this case, however, the meat had been skewered and cooked only to medium-rare. The skewers had dragged contaminants from the meat’s surface down to the center of the kabobs, which hadn’t been cooked to a high enough temperature to kill the bacteria.
Another factor was hand-washing when handling meat — or the lack of it, Rounds said.
“If you think about high school males, they’re probably not the best when it comes to food safety practices,” he said. “So you can have cross-contamination.”
The case is a reminder, Rounds said, that all meat, no matter where it comes from, should be treated with careful precautions.
Rounds JM, Rigdon CE, Muhl LJ, Forstner M, Danzeisen GT, Koziol BS, et al. 2012. Non-O157 Shiga toxin–producing Escherichia coli associated with venison. Emerg Infect Dis http://dx.doi.org/10.3201/eid1802.110855![]()
Abstract
We investigated an outbreak of non-O157 Shiga toxin–producing Escherichia coli at a high school in Minnesota, USA, in November 2010. Consuming undercooked venison and not washing hands after handling raw venison were associated with illness. E. coli O103:H2 and non-Shiga toxin–producing E. coli O145:NM were isolated from ill students and venison.

Freshway Foods has recalled romaine lettuce products sold for food service outlets, wholesale, and in-store retail salad bars and delis after links with over 50 sick people in .jpg) Ohio, Michigan and New York were established. On May 5, 2010, the New York state Public Health Laboratory, Wadsworth Center, in Albany reported finding E. coli O145 in an unopened bag of Freshway Foods shredded romaine lettuce being recalled.
Ohio, Michigan and New York were established. On May 5, 2010, the New York state Public Health Laboratory, Wadsworth Center, in Albany reported finding E. coli O145 in an unopened bag of Freshway Foods shredded romaine lettuce being recalled.
When the recall press release was issued by Freshway Foods around noon today, it said,
The recalled romaine lettuce products were sold to wholesalers and food service outlets in the following states east of the Mississippi river: Alabama, Connecticut, District of Columbia, Florida, Georgia, Illinois, Indiana, Kansas, Kentucky, Maryland, Massachusetts, Michigan, Missouri, New Jersey, New York, North Carolina, Ohio, Pennsylvania, Rhode Island, South Carolina, Tennessee, Virginia, West Virginia, and Wisconsin. The recalled romaine products were also sold for distribution to in-store  salad bars and delis for Kroger, Giant Eagle, Ingles Markets, and Marsh stores in the states listed.
salad bars and delis for Kroger, Giant Eagle, Ingles Markets, and Marsh stores in the states listed.
Amy pointed out, since when in Kansas east of the Mississippi river? Someone else e-mailed me to say the same thing about Missouri. I called Freshway Foods and asked, why are Kansas and Missouri on the list, since they are west of the Mississippi (see, according to their own map, left, the company stops moving product at the river). The U.S. Food and Drug Administration press release about the outbreak repeated the same geographical nosestretcher. Given the states listed, should Dillons supermarket, in Manhattan (Kansas), owned by Kroger, be dumping their salad bar? The dude said, uh, good point, thanks, someone will get back to you.
That person just called, so at least she called back. Unfortunately, she seemed confused (understandable, given the situation, but that’s why everyone in the food system should be prepared for these sorts of things).
The nice lady said, we distribute a few other products into Missouri and Kansas but not romaine lettuce. … Oh, we do send romaine lettuce to a couple of distributors in Kansas City, Missouri.
Sigh.
FDA said today that multiple lines of evidence have implicated shredded romaine lettuce from one processing facility as a source of infections in a multistate outbreak to which this recall may be related.
To date, 19 confirmed cases of E. coli O145 illnesses have been reported from Michigan, Ohio, and New York. These illnesses include 12 individuals who have been hospitalized, .jpg) and three with a potentially life threatening complication called hemolytic uremic syndrome (HUS).
and three with a potentially life threatening complication called hemolytic uremic syndrome (HUS).
The evidence includes preliminary results of product traceback investigations that indicate:
• the shredded romaine lettuce consumed by ill persons in three states originated from one processing facility;
• preliminary results of a case-control study in one state that found a statistically significant association between E. coli O145 infection;
• ingestion of lettuce from the same processing facility; and,
• recovery of E. coli O145 from an unopened package of shredded romaine lettuce from the same processing facility that was obtained from a food service entity associated with the outbreak.
On to the harder questions. Did the contamination occur at the plant (unlikely) or in the field, and where was the stuff grown? It should be easy to figure out where the stuff was grown because, as Freshway proclaims on its website,
We can ensure complete product traceability all the way back to the field. We also exceed the minimum standards with over 30 audits per year conducted on our facilities and growers from firms like Cook and Thurber, Primus, as well as many of our customers’ own quality assurance teams.
Food safety starts on the farm. A table of 34 previous outbreaks involving leafy greens like lettuce and spinach is available at:
http://bites.ksu.edu/sites/default/files/lettuce-outbreaks-table_0.pdf
Misti Crane of the Columbus Dispatch reports this morning that federal health officials will investigate an outbreak of E. coli O145 with cases involving college students in Michigan, New York and Ohio.
Because E. coli O145, a relative of the more common shiga-toxin producing E. coli O157:H7, is not routinely tested for, health types hope an epidemiological  investigation will help pinpoint the suspected food vehicle.
investigation will help pinpoint the suspected food vehicle.
In Feb. 1995, E. coli O111 took the life of a 4-year-old in Australia as part of an outbreak linked to fermented sausage. And in Aug. 2008, E. coli O111 was responsible for hundreds of illnesses and the death of 26-year-old Chad Ingle (right) who had all dined at the Country Cottage restaurant in Locust Grove, Oklahoma.