From a press release, as if you couldn’t tell:
Faculty members from the Kansas State University College of Veterinary Medicine have developed a faster, more efficient method of detecting “Shiga toxin-producing E. coli,” or STEC, in ground beef, which often causes recalls of ground beef and vegetables.
 “The traditional gold standard STEC detection, which requires bacterial isolation and characterization, is not amenable to high-throughput settings and often requires a week to obtain a definitive result,” said Jianfa Bai, section head of molecular research and development in the Kansas State Veterinary Diagnostic Laboratory.
“The traditional gold standard STEC detection, which requires bacterial isolation and characterization, is not amenable to high-throughput settings and often requires a week to obtain a definitive result,” said Jianfa Bai, section head of molecular research and development in the Kansas State Veterinary Diagnostic Laboratory.
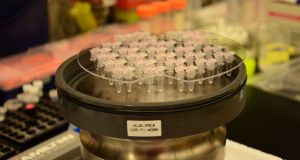
The new method developed by Bai and colleagues requires only a day to obtain confirmatory results using a Kansas State University-patented method with the partition-based multichannel digital polymerase chain reaction system.
“We believe the new digital polymerase chain reaction detection method developed in this study will be widely used in food safety and inspection services for the rapid detection and confirmation of STEC and other foodborne pathogens,” said Jamie Henningson, director of the Kansas State Veterinary Diagnostic Laboratory.
When ingested through foods such as ground beef and vegetables, STEC can cause illnesses with symptoms including abdominal pain and diarrhea. Some illnesses caused by STEC may lead to kidney failure and can be life-threatening.
“Some E. coli strains do not produce Shiga toxins and thus do not affect human health as much,” said Xuming Liu, research assistant professor. “Because cattle feces and ground beef can contain harmless or less pathogenic E. coli along with STEC, the most commonly used polymerase chain reaction cannot identify pathogenic E. coli strains in a complex sample matrix.”
The new digital polymerase chain reaction test was developed for research and food safety inspections that require shorter turnaround and high throughput, without sacrificing detection accuracy.
“While the current, commonly used testing method is considered to be the gold standard, it is tedious and requires many days to obtain results that adequately differentiate the bacteria,” said Gary Anderson, director of the International Animal Health and Food Safety Institute at the K-State Olathe campus.
The study, “Single cell-based digital PCR detection and association of Shiga toxin-producing E. coli serogroups and major virulence genes,” which describes the test design and results, was published in the Journal of Clinical Microbiology.









.jpg) mortality and hemolytic uremic syndrome (HUS) rates observed in healthy adults.
mortality and hemolytic uremic syndrome (HUS) rates observed in healthy adults..jpg) involved in adhesion or invasion.
involved in adhesion or invasion. .jpg) FSIS said in a notice signed by Daniel Engeljohn, assistant administrator for the Office of Policy and Program Development.
FSIS said in a notice signed by Daniel Engeljohn, assistant administrator for the Office of Policy and Program Development. and poultry products are not adulterated as required by the Federal Meat Inspection Act (FMIA) and Poultry Products Inspection Act (PPIA)," Engeljohn wrote.
and poultry products are not adulterated as required by the Federal Meat Inspection Act (FMIA) and Poultry Products Inspection Act (PPIA)," Engeljohn wrote.