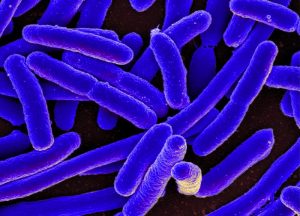
The Norwegian Institute of Public Health has confirmed a genetic match for an infection of E. coli O157 among three children who developed hemolytic uremic syndrome (HUS) this year.
The Institute reported this week,
.jpg)
“The first child became ill in January, the second in February and the third in March. In addition, a sibling of one of the children has also developed HUS, but it has not yet been confirmed whether this is the same bacterial strain.”
One of the four children—all of which are under the age of ten—has died.
The source of the outbreak has yet to be determined. County food safety officials are currently questioning the families of victims on the children’s meals and testing leftover food, while federal officials are seeking information on any further possible cases (i.e. persons, and particularly children, with bloody diarrhea who test positive for enterohemorrhagic E. coli).
I wonder if they’ve looked into the families’ grocery store receipts?
A peer-reviewed article in the April 15 issue of Clinical Infectious Diseases reports that the source of a 2007 outbreak of E. coli in Denmark was found using credit card information.
Investigators had struggled to determine the source of a strain of E. coli O26 that infected 20 Danish children between February and May of 2007.
Flesh and Stone reports that when interviews failed to yield any likely suspect foods, investigators turned to shopping lists.
 “Parents in seven families provided their credit card information and a list of supermarkets where they had shopped. The two supermarket chains that the parents had used most often agreed to help with the investigation. The stores searched their central computers for the precise amount paid and the date and the location of the shop.
“Parents in seven families provided their credit card information and a list of supermarkets where they had shopped. The two supermarket chains that the parents had used most often agreed to help with the investigation. The stores searched their central computers for the precise amount paid and the date and the location of the shop.
“From there, investigators determined that five families had purchased the same brand of fermented, organic beef sausage. A sixth family was linked to the same sausage brand through shopping records provided by the kindergarten attended by two children who became infected with the same E. coli strain, STEC O26. An unopened sample of the sausage also tested positive for the strain.”
Authors of the CID article acknowledged that relying on memory to identify similarities among the diets of outbreak victims diets is often unsuccessful and found credit card information to be “a strong tool in the [current] investigation.”
Investigation of a similar outbreak of E. coli O157 in Iceland successfully used the same method some months later. It could be worth a try for Norway.
 The premise for the project is that affected communities are increasingly recognised as key resources in public health emergencies, and that the concerns and experiences of ordinary people should be harnessed as an important part of the response.
The premise for the project is that affected communities are increasingly recognised as key resources in public health emergencies, and that the concerns and experiences of ordinary people should be harnessed as an important part of the response.






 Belfast City Council staff carried out an inspection of the premises on 19 September, 2008 which uncovered "a number of serious breaches of food hygiene legislation.
Belfast City Council staff carried out an inspection of the premises on 19 September, 2008 which uncovered "a number of serious breaches of food hygiene legislation..jpg)
 “Parents in seven families provided their credit card information and a list of supermarkets where they had shopped. The two supermarket chains that the parents had used most often agreed to help with the investigation. The stores searched their central computers for the precise amount paid and the date and the location of the shop.
“Parents in seven families provided their credit card information and a list of supermarkets where they had shopped. The two supermarket chains that the parents had used most often agreed to help with the investigation. The stores searched their central computers for the precise amount paid and the date and the location of the shop.