Pregnant women are advised to avoid many things, including alcohol, smoking and even their cat’s litter box (what about the refrigerated ready-to-eat foods?). More than 90% of obstetricians and gynecologists in the United States caution patients about handling cat litter during pregnancy, according to a recent survey.
 The reason? A parasite lurking in the pets’ poop.
The reason? A parasite lurking in the pets’ poop.
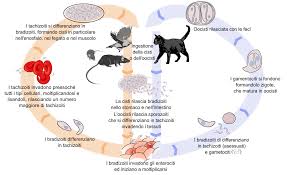
Cats can shed a parasite called Toxoplasma gondii in their feces, and if a pregnant woman accidentally inhales or eats the parasite and becomes infected, there are serious health risks. In 20% to 50% of cases (PDF), the fetus also becomes infected.
Only a very small number of cats are estimated to be shedding these parasites at any time — about 1%, by some estimates — but if a woman is infected within her first trimester, it could lead to microcephaly and other birth defects, as well as an increased risk of mental disability and blindness later in the child’s life.
People with weakened immune systems, such as those who have HIV or are undergoing chemotherapy, can develop neurological problems including headaches and seizures from the infection.
 Other than the groups who were at greater risk, experts had generally thought toxoplasma, or toxo, was of little consequence. But that view started to change in the past decade as reports claimed that the parasite could influence a person’s behavior and even increase the risk of schizophrenia.
Other than the groups who were at greater risk, experts had generally thought toxoplasma, or toxo, was of little consequence. But that view started to change in the past decade as reports claimed that the parasite could influence a person’s behavior and even increase the risk of schizophrenia.
Once a person is infected, toxo lies dormant in their body throughout their life. A recent study found between 10% and 15% of people in the United States to be latently infected with the parasite.
“The consequences of infection with toxo not during pregnancy is all new and not well understood,” said Dr. E. Fuller Torrey, a research psychiatrist at the Stanley Medical Research Institute, a nonprofit organization that supports research on schizophrenia and bipolar disorder.
There have been so many new studies into the link between toxo infection and schizophrenia that Torrey created a web page to keep track of them all. “I’m adding studies almost every month,” he said.
In a 2007 review, Torrey found that people with schizophrenia were 2.7 times more likely to have antibodies against the parasite — which indicate that someone has been infected — than healthy people. This increase in risk would mean that the rate of schizophrenia would increase from 1 in 100 in the general adult population in the United States to 2.7 in 100 among people who have a toxo infection.
A large study by Torrey and his colleagues found that adults who had schizophrenia were more likely to have grown up in homes that had cats, compared with healthy controls. Parents of young children may therefore want to be careful about bringing a new cat into the home.
Despite the evidence found to date, it is still not possible to say whether toxo infections cause these illnesses, said William Sullivan, professor of pharmacology and toxicology, microbiology and immunology at the Indiana University School of Medicine.
Research has merely suggested that people with psychiatric disorders happen to be more likely to have been exposed to toxo. “Correlation plus correlation plus correlation does not equal causation,” Sullivan said.
Sullivan suspects that toxo is not enough on its own to bring on the illness and that another, as yet unknown, risk factor could also be involved.
A good way to find out whether toxo truly causes mental health disorders and changes in behavior would be to give people with schizophrenia a drug that clears their dormant toxo infection and see whether their symptoms improve, Sullivan said. But no such drug exists.
According to Sullivan, there are other ways to become infected with toxo, including eating raw meat, which can harbor the parasite, and gardening or working with soil, where toxo can survive for several years.
A study by Torrey found that there can be 100 toxo spores, or oocysts, under a gardener’s fingernail. Those with a green thumb can take protective steps, such as wearing gloves and a face mask.
People can also become infected by eating the raw meat of animals harboring the parasite. To prevent this, Sullivan advises that people make sure to cook meat thoroughly or else to freeze the meat before eating it.
 Six of the 10 hunters had similar symptoms and illness onset dates. Serologic tests indicated a recent toxoplasmosis infection for all symptomatic hunters, and the risk factor identified was consumption of undercooked deer meat. Among asymptomatic hunters, 2 were already immune to toxoplasmosis, 1 was not immune, and the immune status of 1 remains unknown. Outbreaks of acute toxoplasmosis infection are rare in North America, but physicians should be aware that such outbreaks could become more common.
Six of the 10 hunters had similar symptoms and illness onset dates. Serologic tests indicated a recent toxoplasmosis infection for all symptomatic hunters, and the risk factor identified was consumption of undercooked deer meat. Among asymptomatic hunters, 2 were already immune to toxoplasmosis, 1 was not immune, and the immune status of 1 remains unknown. Outbreaks of acute toxoplasmosis infection are rare in North America, but physicians should be aware that such outbreaks could become more common.